Periodontal disease, generally called gum sickness, encompasses a number inflammatory situations affecting the tissues surrounding and helping the tooth. It is a considerable public fitness difficulty due to its high incidence and ability systemic fitness implications. In Canada, periodontal disorder remains a generic condition, with varying ranges of severity observed across one-of-a-kind demographics.
Prevalence and Impact in Canada
In Canada, the superiority of extreme continual periodontitis is significantly low, affecting less than 10% of the population aged 15 and over.
This statistic positions Canada favorably on the global scale regarding oral fitness. However, despite this exceptionally low incidence, periodontal ailment is still a enormous fitness issue, in particular among middle-aged and aged populations.The disease is characterised through the infection of the helping structures of the tooth, main to symptoms such as gum bleeding, recession, and, in advanced ranges, teeth mobility or loss. Beyond oral fitness, periodontal sickness has been related to systemic conditions, together with cardiovascular disease, diabetes mellitus, and respiration infections. This association underscores the significance of effective control and prevention techniques.
Risk Factors and Etiology
The primary etiological component for periodontal sickness is the buildup of dental plaque—a sticky film of micro organism that forms on tooth. When plaque isn’t successfully removed through regular oral hygiene practices, it may cause irritation of the gums, referred to as gingivitis. If left untreated, gingivitis can development to periodontitis, a extra intense shape of periodontal disease.
Several risk factors make a contribution to the improvement and development of periodontal disorder:
- Smoking: Tobacco use is a prime hazard component, impairing blood float to the gums and hindering recuperation.
- Diabetes Mellitus: Poorly controlled diabetes will increase the risk of infections, consisting of periodontal disease.
- Genetics: Genetic predisposition can impact an person’s susceptibility to periodontal disease.
- Age: The risk increases with age, with a better occurrence found in older adults.
- Socioeconomic Status: Limited get entry to to dental care and decrease socioeconomic fame are associated with better rates of periodontal sickness.
Clinical Manifestations
The medical presentation of periodontal disease varies depending on its severity:
- Gingivitis: Characterized via redness, swelling, and bleeding of the gums, specifically during brushing or flossing.
- Periodontitis: Involves deeper wallet among the tooth and gums, loss of teeth-supporting bone, and capability teeth mobility.
Diagnosis
Diagnosis of periodontal sickness involves a complete medical examination, inclusive of:
- Medical and Dental History: Assessing risk factors and previous dental treatments.
- Clinical Examination: Evaluating the situation of the gums, presence of plaque, and probing depths round teeth.
- Radiographic Assessment: X-rays to assess bone loss and the extent of periodontal involvement.
Management and Treatment
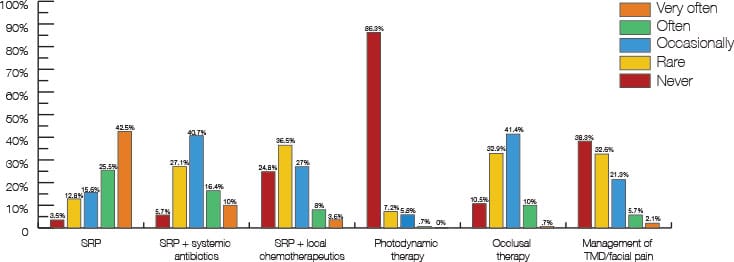
Effective control of periodontal ailment calls for a multifaceted approach:
- Non-Surgical Therapy:
- Scaling and Root Planing: Removal of plaque and tartar from beneath the gum line.
- Antimicrobial Agents: Use of mouth rinses or systemic antibiotics to manipulate bacterial infection.
- Surgical Therapy:
- Flap Surgery: Lifting the gums to remove tartar deposits and decrease pocket depths.
- Bone and Tissue Grafts: Regenerating misplaced bone and tissue to restore periodontal structures.
- Maintenance Therapy:
- Regular Dental Check-ups: Ongoing monitoring and professional cleanings to save you recurrence.
- Patient Education: Emphasizing the significance of day by day oral hygiene practices.
Preventive Strategies
Preventing periodontal ailment includes:
- Oral Hygiene: Brushing at the least twice every day and flossing to remove plaque.
- Regular Dental Visits: Professional cleanings and early detection of periodontal issues.
- Lifestyle Modifications: Smoking cessation and managing systemic situations like diabetes.
Oral Health Disparities in Canada
Despite the general favorable records, disparities exist in oral fitness throughout different populations in Canada. Factors along with socioeconomic repute, geographic vicinity, and get right of entry to to dental care make a contribution to those disparities. Addressing these gaps calls for a concerted effort from healthcare vendors, policymakers, and communities to make certain equitable get admission to to dental care and education.
Conclusion
Periodontal sickness remains a substantial fitness challenge in Canada, with implications extending beyond oral health to typical nicely-being. While the us of a famous favorable records as compared to international requirements, ongoing efforts are essential to preserve and improve oral fitness results. Public fitness initiatives that specialize in prevention, early detection, and equitable get admission to to care are crucial in addressing the load of periodontal sickness in Canada.
